
Straight Tip vs Coude Tip Catheters: Which Is the Right Choice for You?
Millions of people live with urinary incontinence and/or retention issues. To help alleviate symptoms, urologists often prescribe intermittent catheters. Patients will traditionally begin with a straight tip catheter. However, for those who may experience discomfort or regular urinary tract infections, a curved, or coude tip catheter may be the choice
![Logo for Tri-Care insurance [ insurance coverage for medical supplies ]](https://www.rafischer.com/wp-content/uploads/2023/09/ra-fischer-insurance-coverage-home-iontophoresis-hyperhidrosis-urology-supply-catheter-healthcare-4.webp)
![Logo for aetna insurance [ insurance coverage for medical supplies ]](https://www.rafischer.com/wp-content/uploads/2023/09/ra-fischer-insurance-coverage-home-iontophoresis-hyperhidrosis-urology-supply-catheter-healthcare-3-scaled.webp)
![Logo for Cigna insurance. [ insurance coverage for medical supplies ]](https://www.rafischer.com/wp-content/uploads/2023/09/ra-fischer-insurance-coverage-home-iontophoresis-hyperhidrosis-urology-supply-catheter-healthcare-1.webp)
![Logo for Horizon Blue Cross Blue Shield insurance company [ insurance coverage for medical supplies ]](https://www.rafischer.com/wp-content/uploads/2023/09/ra-fischer-insurance-coverage-home-iontophoresis-hyperhidrosis-urology-supply-catheter-healthcare-horizon-bcbs.webp)





![Group of Children playing in the park with bubbles [ RA fischer hyperhidrosis iontophoresis ]](https://www.rafischer.com/wp-content/uploads/2023/09/ra-fischer-iontophoresis-machine-hyperhidrosis-home-medical-supplies-sweating-family-pediatrics-300x169.webp)
![Picture of a patient discussing something with his significant other, holding a pad of paper, dressed professionally [insurance coverage for medical supplies] [ Personalized urology care ]](https://www.rafischer.com/wp-content/uploads/2023/09/ra-fischer-home-medical-supply-iontophoresis-hyperhidrosis-conditions-cancer-neurogenic-bladder-urinary-retention-patient-success-doctor-referral-insurance-6.webp)





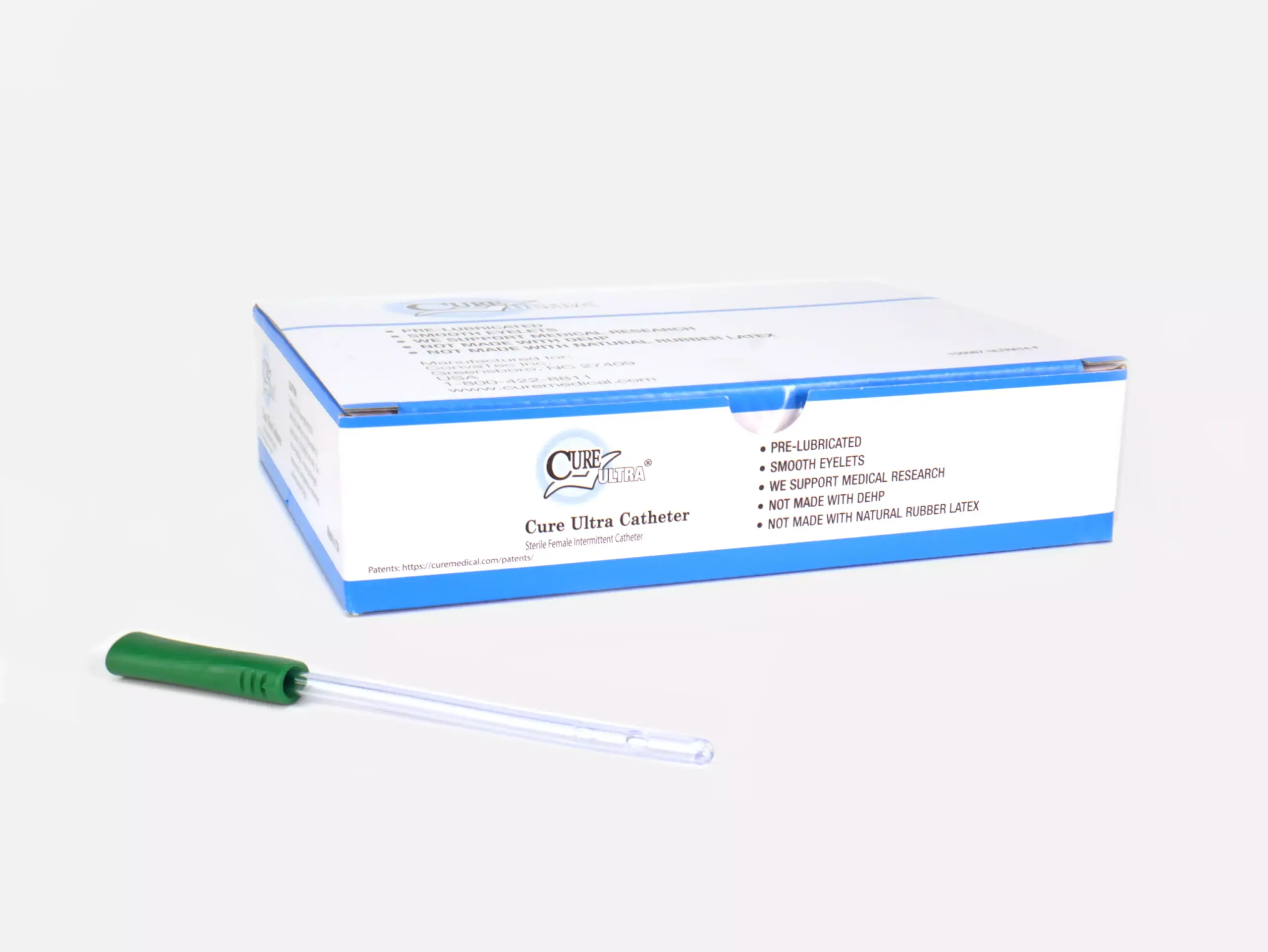
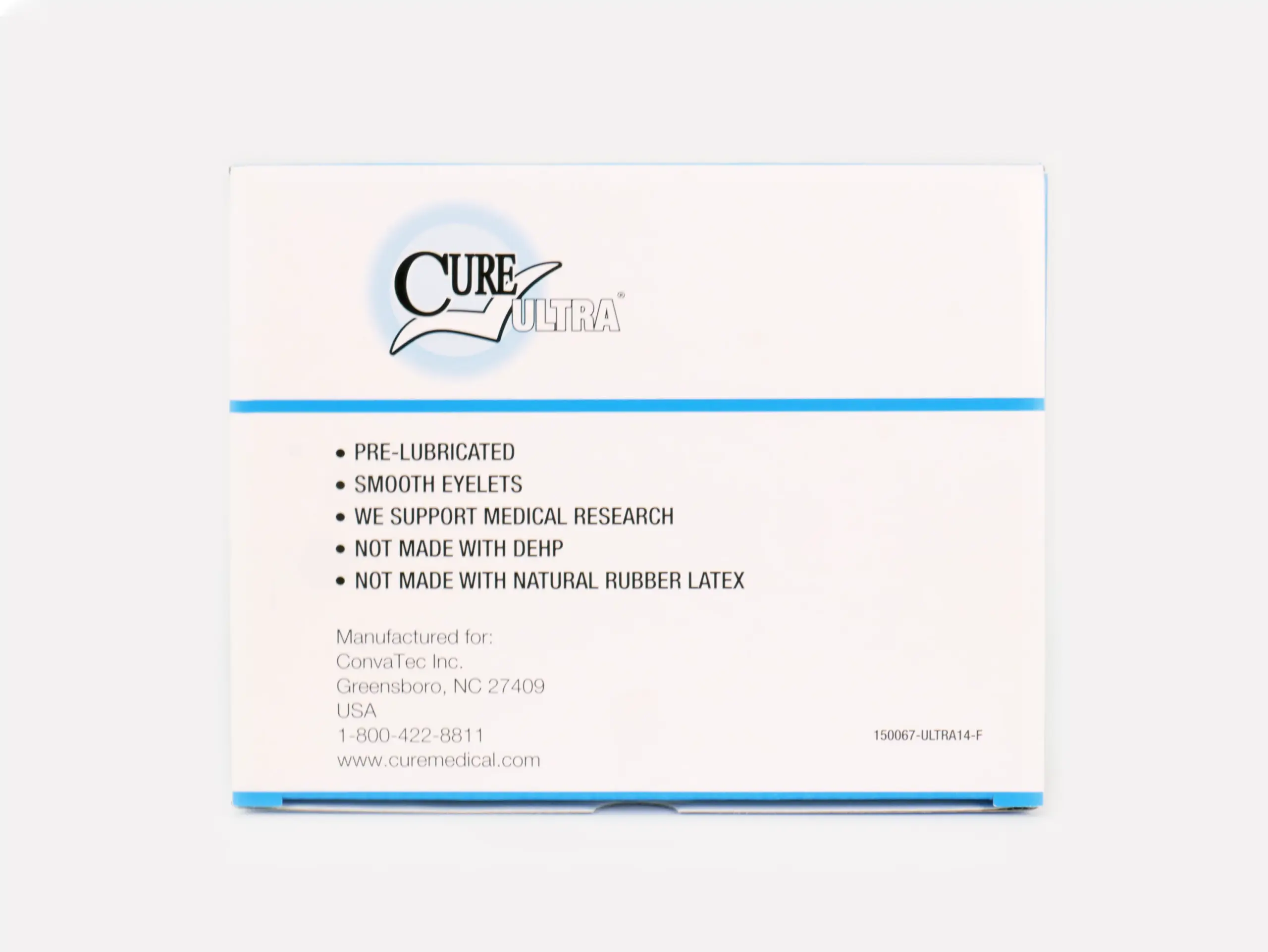
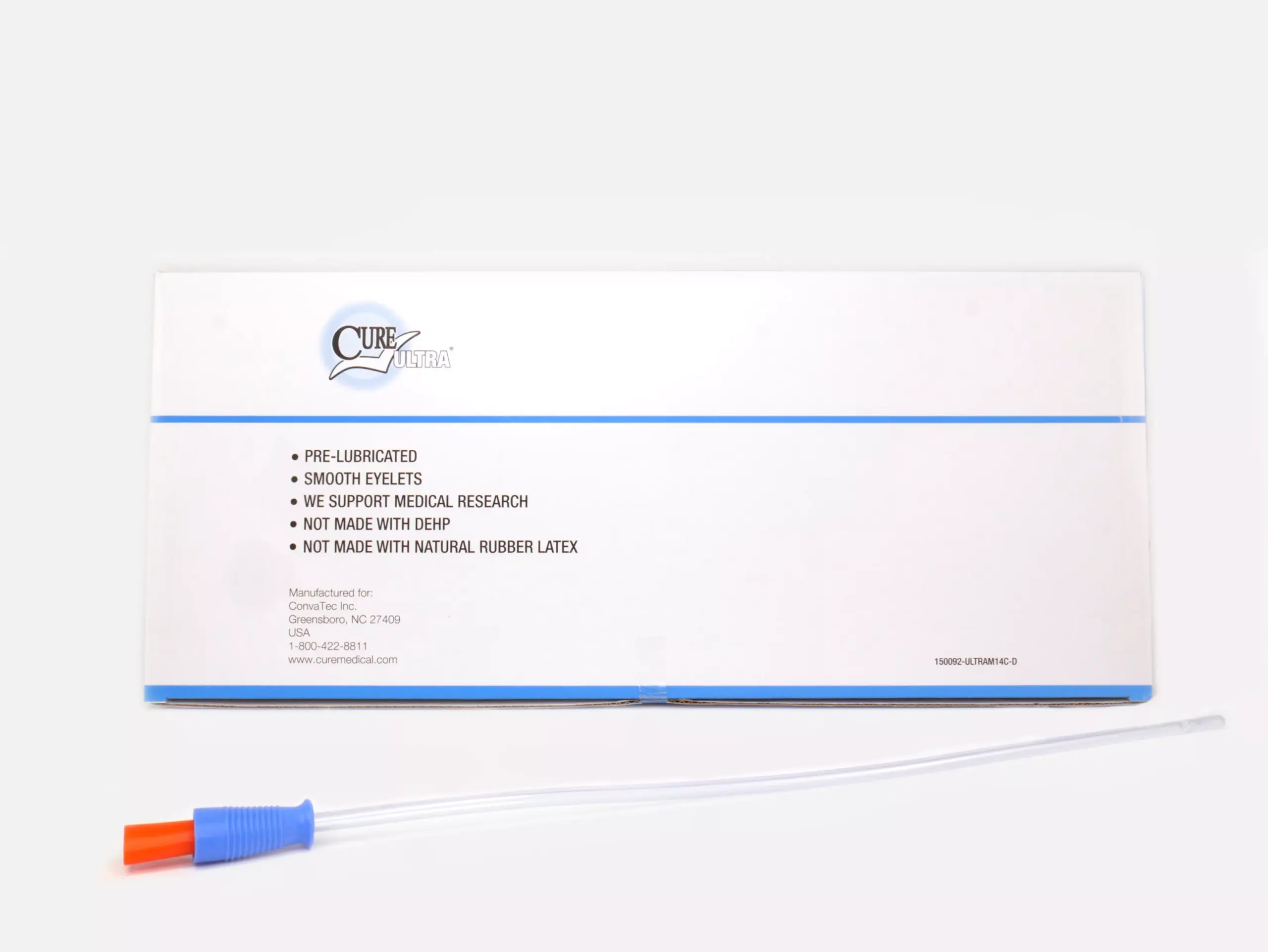
![Photograph of a RA Fischer Co. Cure brand catheter with a green grip, positioned next to a silver-colored water packet, against a white background. [ Personalized urology care ]](https://www.rafischer.com/wp-content/uploads/2023/09/ra-fischer-catheter-urology-supply-healthcare-cure-convatec-hydrophilic-pre-lubricated-insurance-medicare-17-scaled.webp)





![Close-up photograph of one of RA Fischer Co.'s Cure Catheters, closed system, blue [ Personalized urology care ]](https://www.rafischer.com/wp-content/uploads/2023/09/ra-fischer-catheter-urology-supply-healthcare-cure-convatec-hydrophilic-pre-lubricated-insurance-medicare-41-scaled-e1695123684177.webp)